How to Document Your Nursing Shift Like A Boss
Hello Loves!
Documenting your shift in an Electronic Medical Record (EMR) system can be quite intimidating especially when you’re a new nurse or new to the system itself. Don’t fret! It’s easier than you think.
The first tip before we get down to documentation is to have a good assessment sheet where you can document events as you go. Some would say that the assessment sheet is only as good as what you remember, but I’ve always taught students in the past that your assessment sheet acts as your brain. Why need to remember everything when a piece of paper can do it for you? Find a good assessment sheet that works for you and your documentation on the EMR would be easy!
If you’re interested in our free assessment sheet, click here!
Alright let’s get started!
I tell my nurses all the time that documenting your shift is what protects your license. If I perform a chart audit and look through your notes, your note should reflect every single event in a 12-hour timeline. I’m sure you’ve already heard the saying “if it’s not documented, it never happened” all throughout nursing school. I can safely say that this is very much true. Always keep the saying in mind to simply guide what you need to document.
Flowsheets
Your flowsheet is the section where you document your assessments. This section is where you do the most mouse clicking as the findings are already written for you… you just have to choose/click it. There is not much I could show you since the accuracy of your flowsheet is only as good as how you perform your assessment. I can, however, give you some tips to keep in mind so that you not only protect yourself, but also address every aspect of the patients care as much as possible.
What’s good about EMRs is that they usually have a section or page that lists what you’re required to document every shift. However, this is organized and personalized by your institution, therefore, you can easily miss documenting topics that may be important.
Remember the acronym V-PALS for nursing flowsheets…
Vitals | Blood pressure, heart rate, temperature, respiratory rate, and pulse oximetry saturation
This should be documented according to your unit’s protocol whether that be every 4 hours or once a shift.
Pain | Pain assessment and reassessment one hour after every pain medication administration
Pain is technically the 5th vital sign, but it actually expands beyond that. Pain should be assessed and documented every shift, prior to pain medication administration, and one hour after any pain medication administration.
Assessment | Head-to-Toe Assessment
Your head to toe assessment is simply going down from head to toe. I will not list this here as most EMRs have organized this for you respectively. I will elaborate this section a bit more when I go over nursing notes.
LDAs | Lines/Drains/Airway
Lines will include your IV or central lines that enable access to the bloodstream.
Drains will include any line that is not for administration such as foleys, rectal tubes, chest tubes, JP drains, anything that’s draining a body fluid.
Airway will include documenting on oxygen settings and therapies per your unit’s protocol.
Safety & Skin | Safety measures and skin interventions
Safety will include fall interventions, environment checks (patient belongings, medications, etc), safety precautions (isolation, seizure, bleeding risk, etc), and education measures to prevent harm or injury (for eg. teaching patient to call for help using call light before attempting to get out of bed).
Skin interventions is also another precaution but should always be remembered by itself. This is to document turning, repositioning, and other measures to prevent skin breakdown.
Nursing Note Documentation
Your nursing note is more than likely a free form text allowing you to be able to document practically anything you want. This can be a good thing or a bad thing if you don’t have any form of guidance to refer to. Believe it or not… there is such a thing as documenting too much.
My institution allows for us to document anyway we like. I would advise to speak with your nurse leader to discuss how your organization documents. Your nursing note can simply be your head to toe assessment or charting only by exception (see examples below)
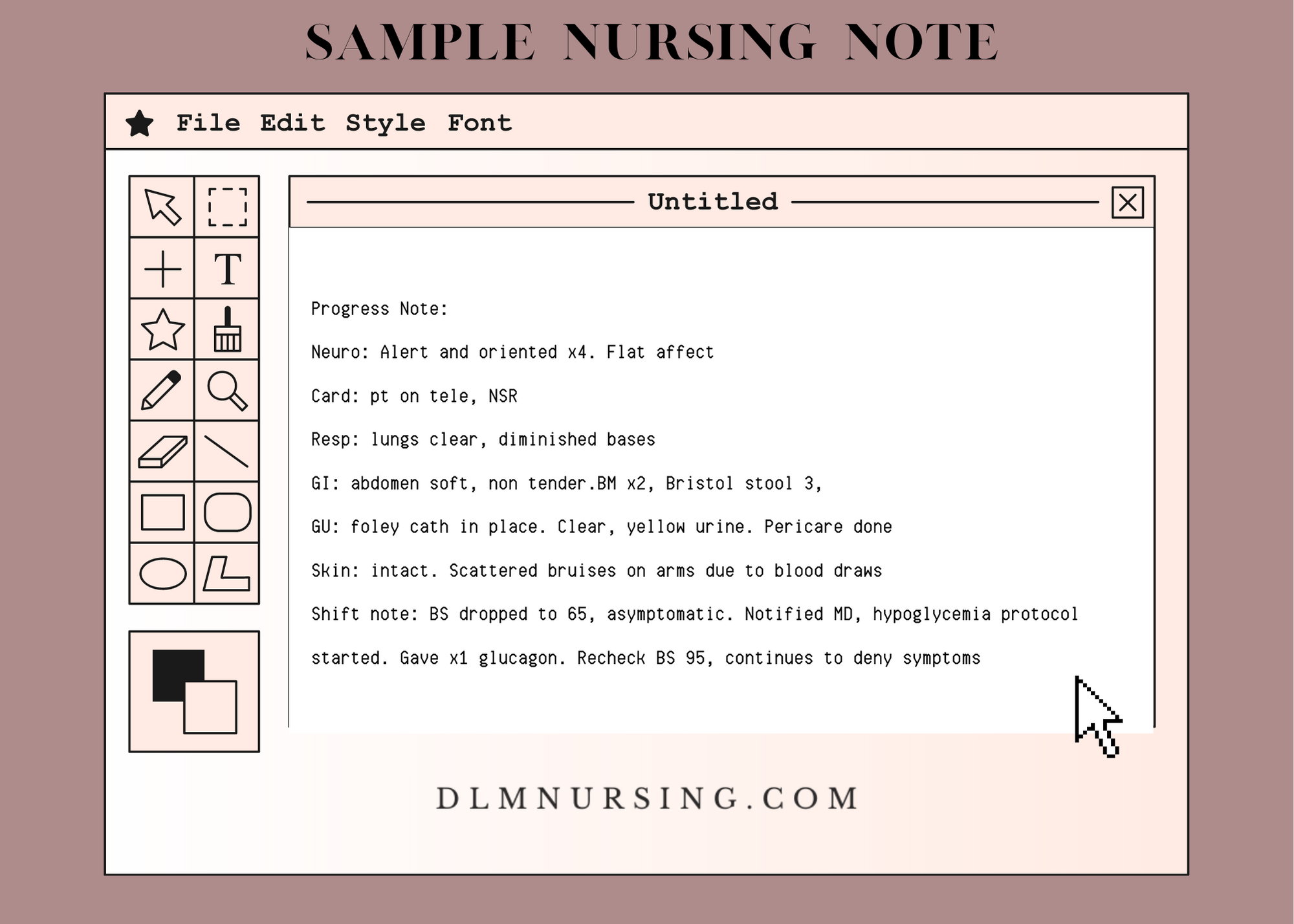
Head to Toe with Event Notes:
This may seem double-charting to some, but you’ll soon realize how inaccessible some flowsheets are. Honestly, it is quite rare for providers to read over flow sheets due to their inability to view them systematically. It is not because they don’t want to read to it. Their EMR view is different from nurses which makes it difficult to see flowsheets. Therefore, I have seen in many institutions where nurses write their head to toe assessments in a simple, organized manner… starting from top to bottom and then ending with a shift note that summarizes the shift with details of significant events such as behavioral events, events with family, notifying providers, etc.
For example:
Neuro: Alert and oriented x4. Flat affect
Card: pt on tele, NSR
Resp: lungs clear, diminished bases
GI: abdomen soft, non tender.BM x2, Bristol stool 3,
GU: foley cath in place. Clear, yellow urine. Pericare done
Skin: intact. Scattered bruises on arms due to blood draws
Shift note: BS dropped to 65, asymptomatic. Notified MD, hypoglycemia protocol started. Gave x1 glucagon. Recheck BS 95, continues to deny symptoms.
Chart by exception:
This simply means you’re documenting only if there’s something to document. If everything is normal, you don’t need to document at all except for care plans. If something is abnormal, you document those details.
Shift note: BS dropped to 65, asymptomatic. Notified MD, hypoglycemia protocol started. Gave x1 glucagon. Recheck BS 95, continues to deny symptoms.
Hope you all enjoyed this post! I hope that you utilize what you all learned here out into the real, nursing world.
Admission Documentation
The nursing admission process is one of the most important pieces of nursing care… this is when a nurse is obligated to gather history and assessment so that it sets up the rest of the inpatient stay for success. How you perform your assessment and gather history will affect your documentation for other providers to see for their own shift.
Whether it be documented in the flowsheet or nursing note, you have to document the following:
Advance Directive
Home/Living status
Recent travel/Travel Screening
Past Medical Health History
Medication List
Assessment
Vitals/Pain with 4 hours of admission
Belongings Check & Securement
Patient Preferences (education/learning style, disability needs, caregiver needs, etc)
Discharge Documentation
Like the admission process, discharging a patient is no easy task, but I can assure you that documenting it is quite simple. Your discharge interventions are usually documented through your progress note by documenting the following:
Education provided
Follow up appointments
Active LDAs that are removed or kept
Mode of transportation
Belongings that are returned
The last tip to documenting like a boss is to remember that Care Plans are mandatory
Did you think you weren’t going to see nursing care plans again? I’m afraid that nursing care plans are not going anywhere.
Remember to keep your care plans individualized to your patient. Do not have a care plan active when it no longer suits the patient. For example, if your patient came in for pain, more than likely you currently have a nursing care plan that pertains to keeping the patient free from pain with active interventions of pain control. But once the pain is resolved, you have to remember to complete this care plan as it no longer pertains to your patient.
The same goes for when your patient develops something new. For example, let’s just say your patient was retaining urine and you had to insert a Foley catheter. You may want to start a whole new care plan on keeping the patient free from infection.
General Tips For EPIC system users:
Utilize smart phrases so that you’re not writing the same thing over and over again
Set specific reminders under your brain section so you don’t forget to document anything
Input flowsheet data into your notes to prevent double documenting
Set a smart phrase to document an admission note and a discharge note
Happy Nursing!
Sincerely,
Dominique Qoraichi, BSN, RN